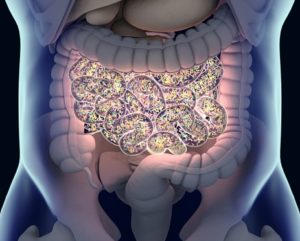
Dietary changes in Western countries, especially the increased consumption of ultra-processed foods, have led to lower fiber intake and higher levels of easily digestible carbohydrates, fats, and additives. These changes disrupt the gut microbiome, causing dysbiosis, which can trigger chronic inflammation and conditions like ulcerative colitis (UC). The gut microbiota ferments dietary fibers to produce short-chain fatty acids (SCFAs), which regulate immune function and maintain gut health. A fiber-deficient diet, common in Western diets, disrupts this process, leading to inflammation and potentially contributing to UC and colorectal cancer. This review examines the complex interactions between diet, the microbiome, and epigenetic changes in UC development.
UC, a chronic colon inflammation, is influenced by genetic factors, environmental influences like diet, and microbiota dysbiosis. The disease has remission and relapse phases, with diet playing a key role in disease management. Western diets, high in fat and sugar, worsen UC by altering the microbiome, leading to excess hydrogen sulfide (H2S) production, which promotes inflammation. Additionally, microbial metabolites can modify gene expression and immune signaling pathways involved in UC. The review emphasizes the importance of understanding how diet and microbial interactions contribute to UC development and the increased risk of colorectal cancer in patients with UC.
Reference: Majumder A, Bano S. How the Western Diet Thwarts the Epigenetic Efforts of Gut Microbes in Ulcerative Colitis and Its Association with Colorectal Cancer. Biomolecules. 2024 May 29;14(6):633. doi: 10.3390/biom14060633. PMID: 38927037; PMCID: PMC11201633.