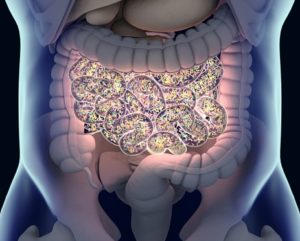
The incidence of inflammatory bowel diseases (IBD), including Crohn’s disease (CD) and ulcerative colitis (UC), is rising in industrialized nations. While IBD’s etiology involves complex interactions between genetics, environmental triggers, and gut microbes, only 19-26% of IBD heritability is explained by genetics. Microbial dysbiosis—alterations in the gut microbiota, such as reduced microbial diversity or blooms of harmful microbes—plays a significant role in IBD progression. Emerging research has identified potential pathobionts, microbes with the capacity to exacerbate inflammation, as contributors to IBD chronicity. These pathobionts, such as Escherichia coli (AIEC), Ruminococcus gnavus, and Candida albicans, exploit inflamed environments to disrupt intestinal barriers, leading to disease flares.
Pathobionts may hinder IBD treatment by promoting resistance to therapies and interfering with microbial treatments like fecal microbiota transplantation (FMT). Identifying these microbes through advanced sequencing and isolating them from inflamed tissues can guide targeted therapies. Promising interventions include using anti-adhesion agents, such as FimH blockers, or phage therapy to selectively eliminate harmful microbes.
Reference: Gilliland A, Chan JJ, De Wolfe TJ, et al. Pathobionts in Inflammatory Bowel Disease: Origins, Underlying Mechanisms, and Implications for Clinical Care. Gastroenterology. 2024 Jan;166(1):44-58. doi: 10.1053/j.gastro.2023.09.019. Epub 2023 Sep 20. PMID: 37734419.