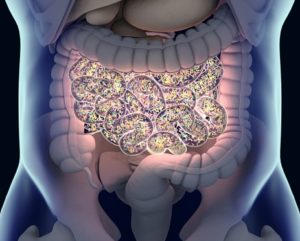
Clostridioides difficile (C. diff) infection remains a major health issue in the US, with severity ranging from asymptomatic carriage to fulminant colitis. Community-acquired cases are rising, while healthcare-associated rates decline. Accurate diagnosis requires clinical judgment alongside tests like GDH, toxin EIA, and NAAT. The 2021 IDSA guidelines recommend fidaxomicin as the first-line treatment for its ability to prevent recurrences, with oral vancomycin as a cost-effective alternative. Treatment plans should be tailored for specific populations, including pregnant patients and those with inflammatory bowel disease.
Preventive measures include minimizing unnecessary antibiotic and proton pump inhibitor use and emphasizing hygiene and contact isolation. Recurrent C. diff, affecting up to 35% of patients, can be treated with fidaxomicin or vancomycin tapers, while fecal microbiota transplantation (FMT) offers high success rates for refractory cases. Adjunctive therapies like bezlotoxumab provide options for high-risk patients but require careful risk assessment. Updated guidelines and evolving C. diff epidemiology underscore the importance of evidence-based practices in improving patient care.
Reference: Wrynn AF. More than a new name: Updates in the management of Clostridioides difficile infection. Nurse Pract. 2024 Aug 1;49(8):14-19. doi: 10.1097/01.NPR.0000000000000209. Epub 2024 Jul 25. PMID: 39049147.