Worldwide, the incidence and prevalence of chronic kidney disease (CKD) continue to increase. One factor contributing to this increase is the increasing incidence of diabetes, a leading cause of CKD. Diabetes and CKD are independent risk factors for kidney failure, and in patients with both diabetes and kidney failure requiring dialysis, the outcomes are particularly poor. Outcomes include microvascular (retinopathy and neuropathy) and macrovascular (peripheral artery disease [PAD], coronary artery disease, and cerebrovascular accidents) complications.
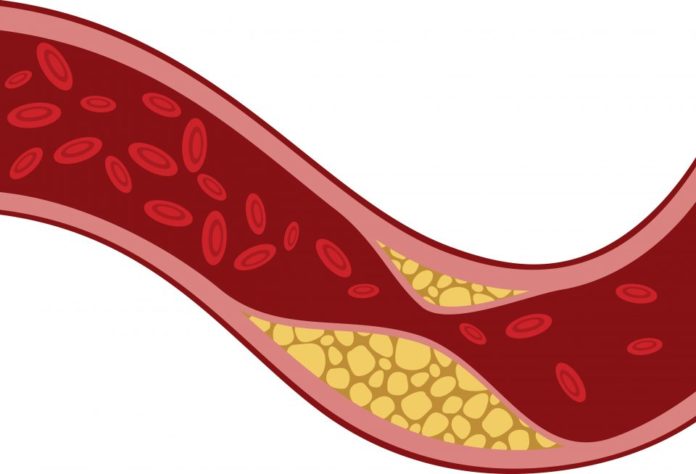
PAD, a pathologic systemic process of arteriolosclerosis and thrombosis leading to a narrowing and eventual occlusion of vessels in the extremities, is common in patients with CKD and is associated with substantial morbidity and mortality as well as increased healthcare costs. According to the US National Health and Nutritional Examination Survey, 10.8% of those with diabetes and 18.2% of those with reduced estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2) have PAD, compared with 3.6% of those without diabetes and 2.8% of those with eGFR at or above that threshold.
In large part, the increased morbidity and costs associated with PAD are linked to its association with foot complications that include neuroischemic foot ulcers, gangrene, infections, and amputations. Limb amputation is an outcome associated with foot ulcers, resulting in patient morbidity and disability and increased costs for the payer.
There have been studies regarding PAD prevalence and lower limb amputations in patients with kidney failure requiring dialysis. However, there are few data on the epidemiology of those diseases in patients with CKD not requiring renal replacement therapy. Information on how PAD or its association with kidney disease influences other adverse health outcomes, such as lower-limb complications.
Mathieu Bourrier, MD, and colleagues conducted a study to compare the prevalence of PAD in patients with CKD and those without CKD and the ways PAD affects the risk for adverse health outcomes, particularly lower-limb complications, cardiovascular events, and survival. Results of the retrospective study were reported in the American Journal of Kidney Diseases [2020;75(5):705-712].
The study exposure was PAD defined by hospital discharge codes and medical claims. Outcomes of interest were all-cause mortality, cardiovascular events, and lower-limb complications, including foot ulcers and nontraumatic amputations. Participants were adult residents of Manitoba, Canada, with at least one serum creatinine measurement between 2007 and 2014.
Following inclusion and exclusion criteria, the final cohort totaled 453,573 individuals. Of those, 4.5% (n=20,600) had a diagnosis of PAD. Those in the PAD group had a greater burden of kidney disease; 30.0% (n=6170) had CKD G-G5 and 3.1% (n=644) had CKD G5D. In the group without PAD, the corresponding values were 10.1% (n=43,395) and 0.4% (n=1926), respectively. Those in the PAD group were older than those without PAD (mean age 69.0 years vs 50.7 years; P<.001). Comorbidity burden, particularly cardiovascular and cerebrovascular disease, was higher in the PAD group than the non-PAD group.
In all analyses, patients without PAD and with estimated glomerular filtration rate ≥60 mL/min/1.73 m2 were the reference group. Proportional hazards models were used to examine the interaction between PAD and level of kidney function (eGFR ≥60 mL/min/1.73 m2, CKD G3-G5, and CKD G5D) for all three adverse outcomes. There was an interaction between PAD and CKD G3-G5 or CKD G5D for lower-limb complications and cardiovascular events, and an interaction between PAD and CKD G3-G5 for all-cause deaths.
Crude rates for lower-limb complications in patients with eGFR ≥60 mL/min/1.73 m2 were 1.0 per 1000 patient-years in patients without PAD versus 9.8 per 1000 patient-years in patients with PAD. Following adjustment for age, sex, and comorbid conditions, there was a 6-fold increased risk in those with PAD compared with those without PAD (hazard ratio [HR], 6.06; 95% confidence interval [CI], 5.41-6.78).
Crude rates for lower-limb complications in patients with CKD G3-G5 were 3.9 per 1000 patient-years in those without PAD and 18.9 per 1000 patient-years in those with PAD. Corresponding HRs were 2.12 (95% CI, 1.89-2.38) and 6.61 (95% CI, 5.74-7.61), respectively. The highest crude rates for lower-limb complications were in patients with CKD G5D (40.5 vs 74.9 per 1000 patient-years in those without and with PAD, respectively. Corresponding HRs were 10.36 (95% CI, 8.83-12.16) and 12.02 (95% CI, 9.58-15.08), respectively.
In patients with eGFR ≥60 mL/min/1.73 m2, the presence of PAD resulted in a nearly 4-fold increase in crude rates of cardiovascular events (13.3 without PAD vs 51.3 with PAD), corresponding to a 56% increased risk for cardiovascular events with PAD versus without PAD (HR, 1.56; 95% CI, 1.49-1.63). In patients with eGFR ≥60 mL/min/1.73 m2, there was a 3-fold increase in crude event rates of morality comparing those without PAD to those with PAD (21.4 vs 70.7 per 1000 patient-years), corresponding to a modestly greater risk in those with PAD versus those without PAD in adjusted model (HR, 1.24; 95% CI, 1.20-1.28).
The researchers cited some limitations to the study results including the use of administrative codes for measurement of outcomes and a limited ability to examine quality-of-care indicators for PAD.
“In conclusion,” the researchers said, “PAD is common in patients with CKD G3-G5 or CKD G5D and is a potent risk factor for cardiovascular events, lower-limb complications, and death. Patients with PAD receiving dialysis should be considered at extreme risk for lower-limb amputation or ulceration, and trials of screening and treatment strategies for these downstream complications should be prioritized in this population.”
Takeaway Points
- Peripheral artery disease (PAD) is common in patients with chronic kidney disease (CKD) and is associated with lower-limb complications and mortality.
- Results of a retrospective cohort study demonstrate that PAD is more common in patients with CKD G3-G5 and G5D compared with those with estimated glomerular filtration rate (eGFR) ≥60 mL/min/1.73 m2.
- Compared with patients with eGFR ≥60 mL/min/1.73 m2 with PAD and without PAD, patients with CKD G5D had 10- and 12-fold higher risks for lower-limb complications, respectively.
Credit: Original article published here.