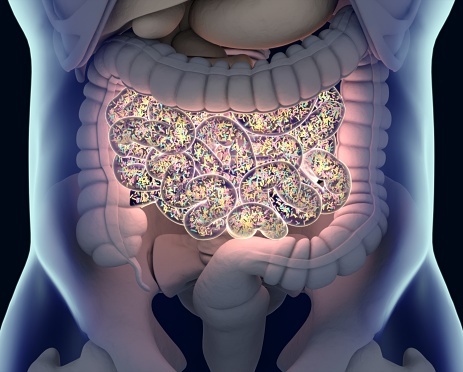
Clostridioides difficile infection (CDI) is a major cause of healthcare-associated diarrhea with high morbidity and mortality. Its spore-forming nature makes prevention and treatment challenging. Diagnosis involves symptom evaluation and a two-step testing approach with glutamate dehydrogenase (GDH) and toxin enzyme immunoassays (EIA). Treatment varies by severity, from fidaxomicin or vancomycin for mild cases to high-dose oral vancomycin with intravenous metronidazole for severe cases.
Advances in CDI management include FDA-approved microbiome-based therapies like SER-109, an oral capsule with Firmicutes spores, and RBX2660, a stool-derived enema, both of which reduce recurrence rates. Fecal microbiota transplantation (FMT) is another option for recurrent cases, though safety concerns remain. Preventative measures such as antibiotic stewardship and infection control are crucial. Emerging therapies like narrow-spectrum antibiotics, microbiome capsules, and potential vaccines offer promising improvements, emphasizing the importance of innovative treatments, accurate diagnostics, and prevention in reducing CDI’s impact.
Reference: Yakout A, Bi Y, Harris DM. Clostridioides Difficile: A Concise Review of Best Practices and Updates. J Prim Care Community Health. 2024 Jan-Dec;15:21501319241249645. doi: 10.1177/21501319241249645. PMID: 38726585; PMCID: PMC11085020.