Patients with prostate cancer who undergo radiotherapy may not have as great of a survival benefit depending on their bone metastasis count and location, according to a study.
The study was a secondary analysis of STAMPEDE, a randomized trial, evaluating those in STAMPEDE’s metastasis M1 radiotherapy comparison. Patients with newly diagnosed metastatic prostate cancer were randomized to receive either standard of care (androgen deprivation therapy with or without docetaxel) or standard of care (SOC) and prostate radiotherapy. The main outcomes were overall survival (OS) and failure-free survival (FFS).
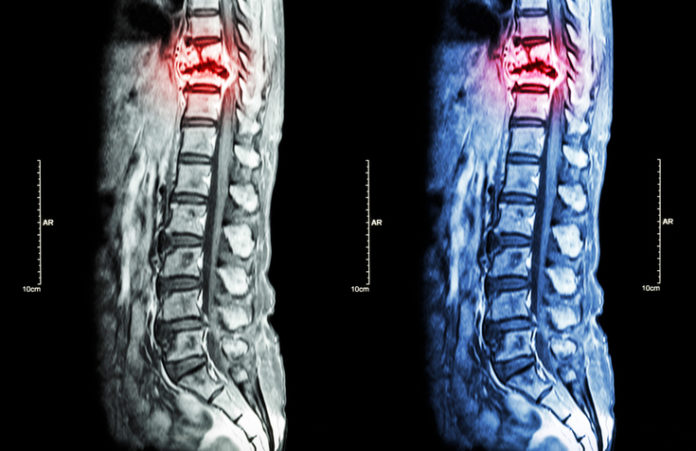
Final analysis included 1,939 men out of 2,061. The median age was 68 years (interquartile range, 63-73 years), and most men had bone metastases (89%). Bone metastasis counts were predictive of OS and FFS benefit from radiotherapy, with survival benefit decreasing as bone metastasis counts increased. The benefit was most significant for those with up to three bone metastases.
Subgroups-based analysis found that the benefit of adding radiotherapy was more significant among patients with only nonregional lymph nodes or fewer bone metastases without visceral metastasis, for both OS (hazard ratio [HR], 0.62; 95% confidence interval [CI], 0.46-0.83) and FFS (HR, 0.57; 95% CI, 0.47-0.70), when compared to patients with at least four bone metastases or any visceral/other metastases, with HRs for OS and FFS of 1.08 (95% CI, 0.91-1.28; P=0.003 for interaction) and 0.87 (95% CI, 0.76-0.99; P=0.002 for interaction), respectively.
“Bone metastatic burden based on conventional imaging is predictive of OS and FFS benefit when prostate radiotherapy is added to SOC in newly diagnosed metastatic prostate cancer. This beneficial effect is most pronounced in patients with up to 3 bone metastases, below which addition of prostate radiotherapy to SOC improves survival in patients without visceral or other metastasis. The criteria for low metastatic burden based on conventional imaging, predictive of survival benefit from prostate radiotherapy in men with newly diagnosed metastatic prostate cancer, should now also include men with M1a disease,” the study authors concluded.
The study appeared in JAMA Oncology.
Credit: Original article published here.