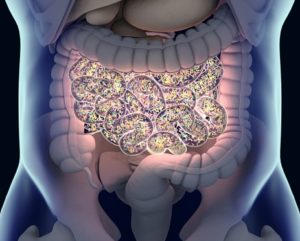
A study focused on understanding the role of mycobiota, particularly fungi and yeasts, in Clostridioides difficile infections (CDI) and colonization (CDC). The research involved analyzing fecal samples from patients with CDI, those asymptomatically colonized with C. difficile, and hospitalized controls without the infection. A key finding was that CDI patients had a significantly higher presence of Candida spp. and Candida albicans but lower levels of Aspergillus spp. and Penicillium spp. compared to CDC patients. No direct link between Clostridioides spp. and fungi was established. Additionally, machine learning analysis indicated that models based on bacterial microbiota data were more effective than those relying on mycobiota or combined microbiota-mycobiota data. The study concluded that while the gut mycobiota composition differs among CDI patients, CDC patients, and controls, it doesn’t directly influence C. difficile and has limited predictive value compared to bacterial microbiota data. The research emphasizes the need for further exploration into the role of specific bacterial genera associated with C. difficile colonization and control groups, potentially aiding in understanding and managing the infection and its colonization.
Reference: Henderickx JGE, Crobach MJT, Terveer EM, et al. Fungal and bacterial gut microbiota differ between Clostridioides difficile colonization and infection. Microbiome Res Rep. 2023 Dec 6;3(1):8. doi: 10.20517/mrr.2023.52. PMID: 38455084; PMCID: PMC10917615.